Ruxolitinib Phosphate: Everything You Need to Know
Ruxolitinib phosphate, a JAK inhibitor, has emerged as a promising therapeutic agent for several blood cancers. It has demonstrated remarkable efficacy in alleviating symptoms and improving survival in patients with myelofibrosis, polycythemia vera, and graft-versus-host disease (GVHD). This article provides an in-depth overview of ruxolitinib phosphate, delving into its mechanism of action, clinical applications, potential side effects, and appropriate dosage regimens.
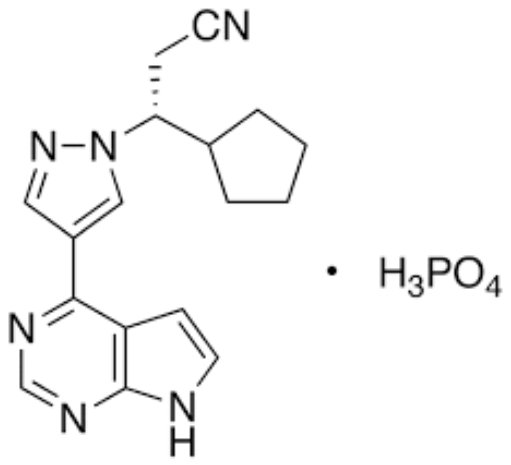
Ruxolitinib Phosphate Mechanism of Action
The mechanism of action of ruxolitinib phosphate involves a multifaceted interplay with various cellular processes:
- Reduced Expression of Pro-Inflammatory Cytokines: JAK signaling plays a crucial role in the production and secretion of pro-inflammatory cytokines, which contribute to the pathogenesis of blood cancers. Ruxolitinib phosphate downregulates JAK signaling, leading to decreased cytokine expression and attenuation of inflammatory responses.
- Downregulation of JAK-STAT Signaling: The JAK-STAT (Janus kinase-signal transducer and activator of transcription) signaling pathway is a critical downstream effector of JAK activation. Ruxolitinib phosphate blocks JAK1 and JAK2, thereby inhibiting the phosphorylation of STAT proteins and disrupting the JAK-STAT signaling cascade.
- Modulation of Cell Cycle Progression: JAK signaling is involved in regulating cell cycle checkpoints, ensuring orderly progression through the cell division process. Dysregulated JAK signaling in blood cancers can lead to uncontrolled cell proliferation. Ruxolitinib phosphate, by inhibiting JAK1 and JAK2, can modulate cell cycle progression, promoting cell cycle arrest or apoptosis in cancer cells.
- Induction of Apoptosis: Apoptosis, programmed cell death, is a crucial mechanism for eliminating damaged or dysfunctional cells. JAK signaling can interfere with apoptosis pathways, allowing cancer cells to evade cell death. Ruxolitinib phosphate, by disrupting JAK signaling, can restore apoptosis mechanisms, leading to the elimination of cancer cells.
The combined effects of ruxolitinib phosphate on these cellular processes contribute to its therapeutic efficacy in treating myelofibrosis, polycythemia vera, and GVHD. By modulating dysregulated JAK signaling pathways, ruxolitinib phosphate can alleviate symptoms, improve survival, and potentially alter the disease course in patients with these blood cancers.
Clinical Applications of Ruxolitinib Phosphate
Myelofibrosis
Myelofibrosis is a chronic blood cancer characterized by bone marrow scarring and reduced blood cell production. This can lead to debilitating symptoms such as fatigue, splenomegaly (enlarged spleen), and pruritus (itching). Ruxolitinib phosphate has demonstrated remarkable efficacy in alleviating these symptoms, improving quality of life, and prolonging survival in patients with myelofibrosis.
Polycythemia Vera
Polycythemia vera is another chronic blood cancer characterized by an overproduction of red blood cells. This can lead to increased blood viscosity, potentially causing cardiovascular complications such as heart attacks and strokes. Ruxolitinib phosphate has been shown to effectively reduce hematocrit levels, alleviate symptoms associated with polycythemia vera, and lower the risk of thrombotic events.
Graft-Versus-Host Disease (GVHD)
GVHD is a serious complication that can arise following allogeneic stem cell transplantation, where donor cells attack the recipient’s tissues. GVHD can manifest in various organs, including the skin, gastrointestinal tract, and liver. Ruxolitinib phosphate has emerged as a valuable treatment option for GVHD, particularly in patients who have not responded adequately to steroids.
In conclusion, ruxolitinib phosphate has revolutionized the treatment landscape for several blood cancers, offering new hope to patients with these challenging malignancies. Its ability to target dysregulated signaling pathways has led to significant improvements in symptom control, survival outcomes, and quality of life. As research continues to expand the frontiers of its therapeutic applications, ruxolitinib phosphate is poised to play an increasingly crucial role in the fight against blood cancers and other diseases.
Side Effects and Contraindications of Ruxolitinib Phosphate
Side Effects
While ruxolitinib phosphate has demonstrated remarkable efficacy in treating various blood cancers, it is essential to be aware of potential side effects. The most common adverse events associated with ruxolitinib phosphate include:
- Hematologic Complications: Ruxolitinib phosphate can affect blood cell counts, potentially causing anemia (low red blood cell count), thrombocytopenia (low platelet count), and neutropenia (low neutrophil count). These side effects are typically manageable with dose adjustments or supportive care.
- Gastrointestinal Adverse Effects: Nausea, vomiting, diarrhea, and abdominal pain are common gastrointestinal side effects associated with ruxolitinib phosphate. These symptoms are usually mild and can be managed with antiemetics and dietary modifications.
- Fatigue: Fatigue is a frequent side effect of ruxolitinib phosphate, often reported by patients with myelofibrosis. Fatigue management strategies, such as adequate rest, exercise modifications, and energy-conserving techniques, can help improve patient well-being.
- Headache: Headaches can occur as a side effect of ruxolitinib phosphate, although they are generally mild and manageable with over-the-counter pain relievers.
- Rash: Skin rash is a potential side effect of ruxolitinib phosphate, typically presenting as a maculopapular rash. Topical corticosteroids can effectively manage skin rash in most cases.

Contraindications
Ruxolitinib phosphate is contraindicated in certain patient populations:
- Severe Liver Impairment: Ruxolitinib phosphate is not recommended for patients with severe liver impairment due to the increased risk of adverse drug reactions.
- Hypersensitivity: Ruxolitinib phosphate is contraindicated in patients with a known hypersensitivity to the drug or any of its components.
- Concurrent Use of Strong CYP3A4 Inhibitors: Ruxolitinib phosphate is metabolized by the CYP3A4 enzyme, and concurrent use of strong CYP3A4 inhibitors can lead to increased drug levels and potential toxicity.
- Pregnancy and Breastfeeding: Ruxolitinib phosphate is not recommended for use during pregnancy or breastfeeding due to potential risks to the developing fetus or nursing infant.
It is crucial to consult with a healthcare professional to determine if ruxolitinib phosphate is an appropriate treatment option and to carefully monitor for potential side effects during therapy.
Dosage and Administration of Ruxolitinib Phosphate
Dosage
The dosage of ruxolitinib phosphate is individualized based on the patient’s age, weight, and the specific blood cancer being treated.
- Myelofibrosis: The starting dose for myelofibrosis is typically 10 mg taken orally twice daily.
- Polycythemia Vera: The starting dose for polycythemia vera is typically 10 mg taken orally twice daily.
- Graft-Versus-Host Disease (GVHD): The starting dose for GVHD is 5 mg taken orally twice daily.
Administration
Ruxolitinib phosphate is available as oral tablets that should be taken with food or milk to enhance absorption. The tablets can be taken with or without water. Patients should avoid taking ruxolitinib phosphate with grapefruit or grapefruit juice, as this can increase drug levels.

Important Considerations
- Adherence to the prescribed dosage and administration schedule is crucial for maximizing the efficacy of ruxolitinib phosphate and minimizing potential side effects.
- Patients should inform their healthcare provider about any other medications, supplements, or herbal remedies they are taking to avoid potential drug interactions.
- Regular follow-up appointments are essential to monitor disease progression, assess treatment response, and manage any side effects that may arise.
- Close monitoring of blood cell counts is necessary to detect and manage potential hematologic complications.
- Patients should promptly report any side effects they experience to their healthcare provider.
Conclusion
Ruxolitinib phosphate, with its targeted mechanism of action and proven clinical efficacy, stands as a beacon of hope for individuals grappling with myelofibrosis and polycythemia vera. As ongoing research continues to unravel the complexities of hematologic disorders, the use of ruxolitinib phosphate represents a significant stride toward personalized and effective treatments. While the medication is not without its challenges, careful monitoring and adherence to prescribed guidelines ensure that the benefits outweigh the potential risks, offering patients a path towards improved quality of life and better disease management.